Sexually transmitted diseases (STDs) can be caused by different types of organisms, including parasites, which often don’t get as much attention as bacterial or viral STDs. These parasitic infections deserve our understanding too, as they can cause significant discomfort and emotional stress if not addressed properly. The good news is that most parasitic STDs respond well to treatment, especially when caught early. Taking care of your sexual health includes being aware of these conditions and knowing when to seek help.
In this post, we’ll explore what parasitic STDs are, their common symptoms, effective treatment options, and practical ways to protect yourself and your partners.
What Are Parasitic STDs?
Parasitic STDs occur when tiny organisms enter your body through sexual contact and essentially “set up camp” there. Unlike bacteria or viruses, these parasites are living creatures that can sometimes survive on bedding, clothing, or other surfaces for short periods. This unique characteristic affects how they spread and how we prevent them. The three main parasitic STDs you should know about include:
- Trichomoniasis (Trich) – This common infection is caused by the parasite Trichomonas vaginalis, which can affect both the genital area and urinary tract
- Pubic Lice (Crabs) – Often called “crabs” because of their appearance, these tiny insects (Pthirus pubis) attach to pubic hair and can cause intense itching
- Scabies – These microscopic mites (Sarcoptes scabiei) burrow under your skin and lay eggs, leading to a characteristic rash and persistent itching, especially at night
Each of these parasitic infections has its own set of symptoms and requires specific treatments, but with proper care, all can be effectively managed.
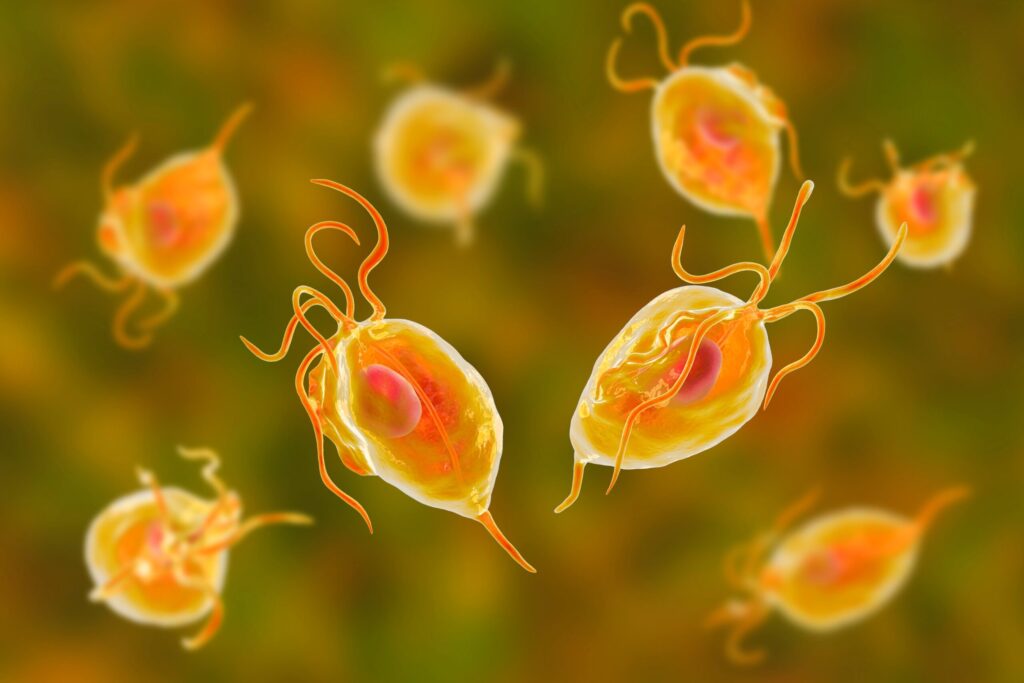
1. Trichomoniasis (Trich)
What Is
Trichomoniasis?
Trichomoniasis, commonly called “trich,” is the most prevalent parasitic sexually transmitted infection. It’s caused by a microscopic parasite called Trichomonas vaginalis. This infection primarily affects the genital area and is typically transmitted through vaginal intercourse, though it can occasionally spread through anal or oral sexual contact as well.
Trichomoniasis Symptoms
Many people living with trichomoniasis don’t experience any symptoms, which unfortunately makes it easy to transmit unknowingly. When symptoms do appear, they typically include:
In Women:
- A yellow-green vaginal discharge that may be frothy and have an unpleasant odor
- Vaginal itching, redness, or general discomfort
- Discomfort during urination or sexual activity
- Inflammation of genital tissues, which can make you more vulnerable to other STIs, especially HIV
In Men:
- Burning feelings when urinating or ejaculating
- Discharge from the penis
- Discomfort or irritation inside the penis
Causes and Transmission
Trichomoniasis develops from infection with the parasite Trichomonas vaginalis. This parasite typically passes from one person to another during sexual contact. This transmission commonly occurs during vaginal, anal, or oral sexual activities. Sharing sex toys that haven’t been properly cleaned can also spread the infection.
One of the biggest challenges in preventing trichomoniasis is that many people don’t show any signs of infection. In fact, research suggests up to 70% of people with trichomoniasis don’t experience symptoms, making it difficult to detect and easy to pass on to partners without realizing it.
Transmission can happen even without penetrative sex. Activities like genital touching or oral sex still carry risks. However, you can’t get trichomoniasis through casual, non-sexual contact such as sharing meals or drinks, kissing, or holding hands.
Diagnosis and Treatment
Healthcare providers diagnose trichomoniasis through laboratory testing, including:
- Looking at a sample of vaginal fluid or urethral discharge under a microscope
- Quick antigen tests or nucleic acid tests
The good news is that trichomoniasis is easily treatable with oral antibiotics, typically metronidazole or tinidazole. For best results, all sexual partners must receive treatment at the same time to prevent passing the infection back and forth.
Risks of Untreated Trichomoniasis
If you don’t get treatment for trichomoniasis, several health concerns may develop:
- Higher chances of acquiring or transmitting HIV
- Complications during pregnancy, including premature delivery and babies with low birth weight
- Ongoing irritation and discomfort that affects your quality of life
Trichomoniasis and Pregnancy
For expectant mothers, trichomoniasis poses serious concerns. Pregnant women with this infection face an increased risk of delivering their babies too early, which can lead to various health challenges for newborns. Additionally, babies born to mothers with trichomoniasis are more likely to have lower birth weights, which brings additional health risks.
The infection may also contribute to other pregnancy complications like preterm labor and early rupture of the amniotic sac. In more severe cases, trichomoniasis might increase the risk of pregnancy loss.
Because of these potential complications, it’s especially important for pregnant women to be tested for trichomoniasis and other sexually transmitted infections. Fortunately, treatment is generally considered safe during pregnancy and can help protect both mother and baby from these negative outcomes.
Risk Factors and Groups Affected
Certain populations have higher rates of trichomoniasis infection. These include:
- Sexually active individuals: Anyone engaging in sexual activity faces some risk, particularly those with multiple partners or who don’t consistently use barrier protection.
- Women: Women experience trichomoniasis infections more frequently than men, especially those with multiple partners or inconsistent condom use.
- Older women: The risk tends to increase with age, particularly for women with multiple sexual partners or inconsistent protection practices.
- African American women: Studies show African American women experience higher rates of trichomoniasis compared to white or Hispanic women, particularly when other risk factors are present.
- People living with HIV: Individuals who have HIV may be more vulnerable to trichomoniasis and other STIs, especially with multiple partners or inconsistent protection.
For people in these higher-risk groups, regular screening for trichomoniasis and other STIs is an essential part of maintaining sexual health and preventing complications. Remember, many STIs don’t cause noticeable symptoms, so testing is the only way to know your status with certainty.
2. Pubic Lice (Crabs)
What Are Pubic Lice?
Pubic lice, commonly known as “crabs”, are tiny insects (Pthirus pubis) that infest pubic hair and feed on blood. They are different from head lice and body lice, as they have claws adapted to grip coarse pubic hair.

Symptoms of Pubic Lice
Symptoms typically develop within a few days to a few weeks after infestation and include:
- Intense itching in the pubic area
- Red or blue bite marks on the skin
- Small white or yellow lice eggs (nits) attached to hair
- Visible crawling lice
How Are Pubic Lice Spread?
Pubic lice are most commonly spread through:
- Sexual contact (even without penetration)
- Shared clothing, towels, or bedding
Diagnosis and Treatment
Diagnosis is usually made through visual inspection of lice and eggs in the pubic area.
Treatment:
- Over-the-counter or prescription topical treatments, such as permethrin lotion or pyrethrin-based shampoos
- Washing all bedding, clothing, and towels in hot water
- Combing out nits with a fine-toothed comb
Risks of Untreated Pubic Lice
Although pubic lice do not transmit diseases, untreated infestations can lead to:
- Secondary bacterial infections from scratching
- Skin irritation and inflammation
- Psychological distress and embarrassment
3. Scabies
What Is Scabies?
Scabies is caused by the mite Sarcoptes scabiei, which burrows into the skin and lays eggs, leading to severe itching and skin irritation. It is spread through prolonged skin-to-skin contact, including sexual contact.
Symptoms of Scabies
Symptoms typically appear 4 to 6 weeks after infestation and include:
- Intense itching, especially at night
- Small red bumps or blisters, often in clusters
- Thin, wavy, grayish-white burrow tracks on the skin
- Commonly affected areas: genital region, hands, wrists, armpits, elbows, and between fingers
Diagnosis and Treatment
Scabies is diagnosed through:
- Visual examination of the skin
- Skin scrapings examined under a microscope to detect mites
Treatment:
- Prescription topical treatments, such as permethrin cream or ivermectin
- Washing clothing, bedding, and towels in hot water
- Treating all household members to prevent re-infestation
Risks of Untreated Scabies
If untreated, scabies can cause:
- Severe skin infections due to excessive scratching
- Thickened, scaly skin in chronic cases (Norwegian scabies)
- Spreading to others in close contact
How to Prevent Parasitic STDs
Prevention strategies for parasitic STDs include:
- Safe sex practices: Use condoms and limit sexual partners.
- Personal hygiene: Avoid sharing clothing, towels, and bedding.
- Regular screenings: Get tested if you experience symptoms or have multiple partners.
- Awareness: Learn to recognize symptoms and seek treatment promptly.
- Treatment for both partners: Ensure both the infected individual and their sex partner receive treatment to prevent reinfection.
Conclusion
Parasitic STDs like trichomoniasis, pubic lice, and scabies can cause significant discomfort but are treatable. Practicing safe sex, maintaining good hygiene, and seeking prompt treatment can help prevent and manage these infections. If you suspect you have a parasitic STD, consult a healthcare provider for diagnosis and treatment. By staying informed and proactive, you can protect yourself and your partners from these unwelcome invaders.
FAQ
Can you get a parasitic STD from oral sex?
Trichomoniasis is a sexually transmitted infection primarily transmitted through vaginal sex, though it is possible but rare to contract it through oral sex. Pubic lice and scabies can spread through close physical contact, including nonsexual interactions.
Do condoms prevent parasitic STDs?
Condoms can help reduce the risk of trichomoniasis but may not fully prevent pubic lice or scabies, as these parasites can infest areas not covered by condoms.
How long can pubic lice live without a human host?
Pubic lice can survive for about 24-48 hours without a human host. They can be spread through infested bedding, clothing, or towels.
Can scabies go away on its own?
No, scabies will not go away without treatment. Prescription creams or oral medications are needed to eliminate the mites.
Is trichomoniasis a serious STD?
Trichomoniasis is usually not life-threatening, but it can cause discomfort and increase the risk of other infections, including HIV, if left untreated.
Sources:
CDC. About Trichomoniasis. https://www.cdc.gov/trichomoniasis/about/index.html
National Library of Medicine. Trichomoniasis and adverse birth outcomes: a systematic review and meta-analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC9704755/
NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/sexual-and-reproductive/pubic-lice/
World Health Organization. https://www.who.int/news-room/fact-sheets/detail/scabies