Yeast infection vs chlamydia: knowing the difference is important for diagnosis and treatment. Both share symptoms like itching and discharge but need completely different therapies. This guide helps you identify, differentiate, and understand how to treat these conditions.
Key Takeaways
- Yeast infections and chlamydia share similar symptoms, but the treatments differ. You need to properly diagnose both conditions for effective treatment and to avoid complications.
- Yeast infections are caused by fungal overgrowth and are not sexually transmitted, while chlamydia is a bacterial STI primarily spread through sexual contact.
- Timely medical intervention is crucial, as untreated yeast infections can lead to chronic discomfort, and untreated chlamydia can result in severe health complications, including infertility.
Understanding Yeast Infections and Chlamydia
If you have symptoms such as itching, irritation, or abnormal discharge, it can be confusing to determine whether these signs indicate a yeast infection or possibly something more serious like a sexually transmitted disease (STD). Since numerous STDs present similar symptoms to those of yeast infections, identifying the precise cause usually requires expertise from a medical professional. It’s important to get an accurate diagnosis before beginning treatment.
Let’s explore each of these conditions so you know how to recognize you may have an issue:
What is a Yeast Infection?
A vaginal yeast infection is a fungal infection caused by the excessive multiplication of Candida albicans, a fungus which typically resides in the vagina. This condition can be triggered by factors such as hormonal imbalances, antibiotic usage, and specific medications that lead to an increase in this fungus. The symptoms experienced during a yeast infection consist of:
- Severe vaginal itching
- Irritation
- Discharge (Yeast Infection discharge is usually thick and has an appearance similar to cottage cheese)
About 75% of women of childbearing age will experience at least one instance of a yeast infection over their lifetimes. Despite being associated with intimate areas, a yeast infection is not the same as an Sexually Transmitted Disease, as they are caused by an overgrowth of a vaginal fungus (similar to Bacterial Vaginosis, another form of vaginal infection).
What is Chlamydia?
Chlamydia, a sexually transmitted infection (STI) of bacterial origin, results from the bacteria Chlamydia trachomatis. This infection is particularly prevalent within the demographic aged 15 to 25 years, with an estimated rate of 48% of all cases. Often presenting no symptoms for extended durations, those infected with chlamydia may inadvertently transmit the disease to their sexual partners, thereby increasing the incidence of sexually transmitted infections.
Transmission Methods
Recognizing the transmission methods for both yeast infections and chlamydia is crucial to prevent them effectively. Most yeast infections arise from a range of causes, such as fluctuations in hormone levels or the use of antibiotics, whereas std’s spreads primarily through sexual activity.
Let’s delve into how chlamydia and yeast infections spread.
How Yeast Infections Spread
Hormonal changes, like those during pregnancy or menopause, can lead to yeast infections. Antibiotics taken in excess may also upset the vaginal bacterial equilibrium and foster yeast proliferation. Stress, weakened immune systems, and inadequate hygiene are additional factors.
How Chlamydia Spreads
Chlamydia can be spread by being sexually active with an infected partner, encompassing vaginal, anal, and oral sex. The likelihood of transmitting this infection can be greatly diminished by regularly using barrier protection such as condoms, so having chlamydia does not mean you have to stop being sexually active.
Recognizing Symptoms
Recognizing the signs of yeast infections and chlamydia can be challenging since they share similarities with other conditions affecting vaginal health. Each can result in itching and abnormal vaginal discharge, complicating the diagnosis without expert consultation.
Despite these similarities, unique symptoms exist that may aid in distinguishing one from the other.
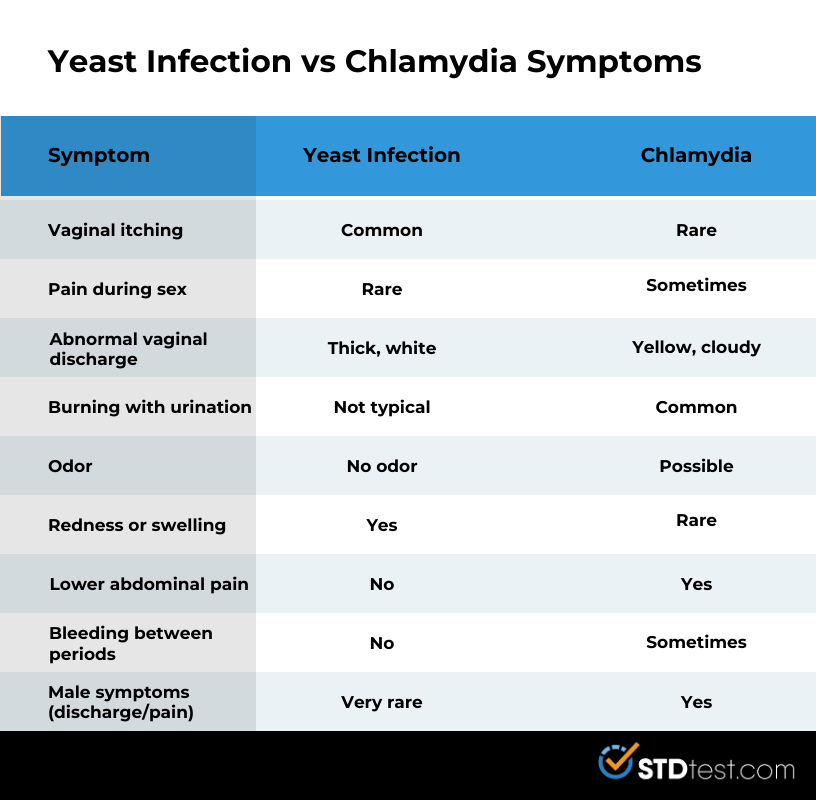
Symptom | Yeast Infection | Chlamydia |
|---|---|---|
| Vaginal itching | ✅ Common | ❌ Rare |
| Pain during sex | ❌ Rare | ✅ Sometimes |
| Abnormal vaginal discharge | ✅ Thick, white | ✅ Yellow, cloudy |
| Burning with urination | ❌ Not typical | ✅ Common |
| Odor | ❌ No odor | ✅ Possible |
| Redness or swelling | ✅ Yes | ❌ Rare |
| Lower abdominal pain | ❌ No | ✅ Yes |
| Bleeding between periods | ❌ No | ✅ Sometimes |
| Male symptoms (discharge/pain) | ❌ Very rare | ✅ Yes |
Symptoms of Yeast Infections
The onset of a vaginal yeast infection presents with itching and inflammation around the entrance to the vagina, often accompanied by vaginal burning. A hallmark indicator is the appearance of copious, white discharge that bears a resemblance to cottage cheese. The discharge associated with a yeast infection might also emit an unpleasant odor.
Should you encounter symptoms similar to those of a yeast infection, it’s important to reach out to a medical professional. It’s especially critical to seek healthcare advice if you’re experiencing new vaginal pain, elevated body temperature, atypical bleeding patterns, or if you have severe symptoms. Proper diagnosis is key for effective management and treatment of the condition, as neglecting care can lead to severe health problems..
Symptoms of Chlamydia
Chlamydia is frequently known as a ‘silent’ infection due to its propensity to occur without any noticeable symptoms. When symptoms are present, they can manifest as minimal itching and the presence of discharge that may emit an unpleasant odor, similar to a fishy smell. White, green, and yellow discharge are all common colors of chlamydia discharge. Chlamydia can also cause burning or pain during urination or sex.
Diagnosis Methods
For effective treatment of yeast infections and chlamydia, it is crucial to diagnose these conditions accurately. Healthcare professionals rely on both physical examinations and lab tests to identify these issues with precision.
Let’s look at methods used for diagnosing yeast infections vs. chlamydia.
Diagnosing Yeast Infections
Laboratory tests and physical assessments are often used to diagnose yeast infections. Confirmation typically involves taking a vaginal swab for microscopic analysis to detect Candida.
Diagnosing Chlamydia
Nucleic acid amplification testing (NAAT) is the most common technique for identifying chlamydia, utilizing either urine tests or swab assessments. To conduct these tests, samples such as first-catch urine and vaginal swabs are collected. Rectal and throat swabs may be collected from certain populations that have a higher risk.
Treatment Options
Administering the correct treatment upon diagnosis of either yeast infections or chlamydia is essential in ensuring proper care. Antifungal medications are commonly used to treat yeast infections, while antibiotics are necessary for the treatment of chlamydia.
Just as symptoms differ, so do treatments.The distinct treatments for each condition are outlined as follows:
Treating Yeast Infections
Creams, ointments, or vaginal supplements that contain antifungal medication are typically employed to combat yeast infections. These drugs represent the principal method of managing Candida-related ailments. The duration of yeast infection treatment may take up to two weeks. In cases of intense candidiasis, more complex treatment strategies might be needed.
Alongside antifungal treatment for Candida infections, probiotics like lactobacilli are often suggested to support recovery. Should symptoms persist despite over-the-counter remedies, obtaining additional consultation is critical.
Treating Chlamydia
Chlamydia often requires a single dose of antibiotics or a 7-day course. Side effects of chlamydia treatment may include stomachache, diarrhea, or a vaginal yeast infection. Patients are advised to refrain from sexual activity until treatment is complete.
Treating sexual partners helps prevent reinfection. Following the treatment plan guarantees effective eradication of the infection.
Potential Complications
Neglecting to address yeast infections and chlamydia can result in severe health issues. Untreated infections may cause persistent pain, repeated occurrences of infection, and complications that can greatly diminish one’s well-being.
Risks of Untreated Yeast Infections
If yeast infections are not treated over an extended period, they can cause ongoing discomfort and repeat flare-ups. These chronic or unaddressed infections might lead to the development of painful sores in the genital area as well as other complications that could necessitate professional medical care. Persistent yeast infections may result in inflammation, tenderness, and skin conditions affecting the vaginal region.
When left untreated for a considerable duration, yeast infections have the potential to weaken the immune system. A weak immune system raises the risk of transmission.
Risks of Untreated Chlamydia
If not addressed promptly, chlamydia can lead to several severe consequences such as:
- The development of pelvic inflammatory disease (PID)
- An increased risk of infertility and ectopic pregnancy.
- The potential spread from an infected mother to her baby during birth, which could result in significant health problems for the infant
- Reactive arthritis that may cause persistent pain in the joints
An untreated chlamydia infection is capable of causing scarring within the reproductive organs, which may result in ongoing pelvic discomfort and PID. Neglecting to treat chlamydia increases one’s susceptibility to other sexually transmitted infections (STIs), including HIV.
Prevention Strategies
Prevention is always better than a cure. Preventive measures can significantly lower the risk of chlamydia and yeast infections.
Preventing Yeast Infections
Maintaining proper hygiene can aid in averting mild yeast infections. Adhering to the following guidelines is advisable:
- Cleansing the vaginal region daily using gentle, fragrance-free soap
- Opting for airy cotton undergarments
- Selecting clothes that are loose-fitting to decrease moisture buildup
- Swiftly changing out of wet attire after engaging in activities such as swimming or working out
By adopting these habits, you’re likely to lessen your chances of developing yeast infections.
Dietary changes can also help avoid developing a yeast infection. To help prevent or address yeast infections, it’s beneficial to consume a diet that is low in processed flours and sugars, free from yeasts and dairy products. These dietary adjustments contribute to maintaining good vaginal health and preventing frequent occurrences of yeast infections.
Preventing Chlamydia
Practicing monogamous relationships and informing recent sexual partners if diagnosed with chlamydia are crucial steps in prevention. Safe sex practices, including consistent condom use and regular STI testing, are essential for preventing chlamydia. Simultaneously treating sexual partners will also prevent reinfection.
When to Seek Medical Help
Self-diagnosis of yeast infections is often inaccurate, and consulting a healthcare provider is recommended for proper diagnosis and treatment.
Signs You Need a Doctor
Seek medical attention for:
- Persistent vaginal pain or discomfort that is new or has worsened
- Abnormal symptoms like bleeding or fever accompanying vaginal symptoms
- Increased discomfort during urination or sexual activity
These symptoms necessitate a consultation with a doctor.
Summary
Understanding the differences between chlamydia and yeast infections is vital for effective treatment and prevention. Recognizing symptoms, knowing how these conditions spread, and understanding the importance of proper diagnosis can empower you to take control of your vaginal health. By adopting preventive measures and seeking timely medical help, you can avoid complications and ensure a healthier future.
FAQs
What are the main differences between chlamydia and yeast infections?
The main difference between chlamydia and yeast infections is that yeast infections are caused by an overgrowth of Candida fungus and are not sexually transmitted, whereas chlamydia is a bacterial sexually transmitted infection caused by Chlamydia trachomatis.
How can I prevent yeast infections?
To prevent yeast infections, prioritize good hygiene, wear breathable clothing, avoid irritants, and maintain a healthy diet while ensuring you change out of damp clothing promptly.
What are the treatment options for chlamydia?
Chlamydia can be effectively treated with antibiotics such as Azithromycin or Doxycycline. It is essential for sexual partners to be treated as well to prevent reinfection.
What should I do if I experience symptoms of a yeast infection or chlamydia?
If you experience symptoms of a yeast infection or chlamydia, it is essential to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
What are the risks of leaving chlamydia untreated?
Neglecting to treat chlamydia can lead to severe complications such as pelvic inflammatory disease, increased risk of infertility, persistent pain in the pelvic region, and a heightened chance of acquiring additional sexually transmitted infections (STIs), including HIV.
Sources:
Center for Disease Control (CDC). National Overview of STIs. https://www.cdc.gov/sti-statistics/annual/summary.html
Mayo Clinic. Yeast Infections. https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999
Office on Women’s Health. https://womenshealth.gov/a-z-topics/vaginal-yeast-infections
Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/4023-chlamydia
