Did you know that Gonorrhea, one of the most common sexually transmitted infections, has a nickname that sounds like something out of a medieval tavern? The term “The Clap” has puzzled many and invites curiosity about its origins and meaning. Understanding this term requires exploring both its linguistic roots and the historical context surrounding the treatment of gonorrhea.
Gonorrhea itself is a bacterial infection caused by Neisseria gonorrhoeae, and it has affected countless individuals globally for centuries. In the United States alone, the CDC reported over 600,0000 cases in 2023. Symptoms can vary significantly between genders, often leading to misunderstandings and stigmas that further complicate the conversation around sexual health.
In this article, we will unravel the origins of the nickname “the clap,” define gonorrhea and its symptoms, and explore its transmission and treatment options.
Gonorrhea is known by the std slang term “the clap” or “the drip”. This STI can infect the reproductive organs, throat, and eyes. Common symptoms are sore throat, painful urination, and pus-like discharge. The nickname’s origins remain somewhat unclear, but there are popular theories explaining how this term came to be associated with gonorrhea.
Linguistic Roots of the Nickname “The Clap”
One theory is that “the clap” comes from the Old English word clappan, which means “to throb” or “to beat”. This fits with the throbbing pain of a gonorrhea infection in the genitals. When left untreated gonorrhea can cause inflammation and discomfort; early sufferers may have described the pain as “clapping”. This etymology suggests pre-moderns named their diseases after its symptoms.
Another theory is that the term comes from the medieval era when brothels were called “clap houses”. These were the places where STIs were most commonly transmitted. The association between brothels and gonorrhea might have led to “the clap” as a shorthand for the infection you got in such places.
A more gruesome and unpleasant theory is that the term comes from an early treatment for gonorrhea. Physicians or sufferers would “clap” or slap the penis between two hands or against a hard object to expel the discharge. This was thought to relieve symptoms by forcing the pus out of the urethra. This was not based on medical science and probably did more harm than good but shows the desperation of the times when there was no treatment and may have contributed to the name of the disease.
While the exact origin of “the clap” remains unclear, these explanations collectively shed light on the interplay between language, medicine, and societal attitudes toward sexually transmitted infections throughout history, and may give us some insight to where the nickname originated.
Historical Treatments and Methods
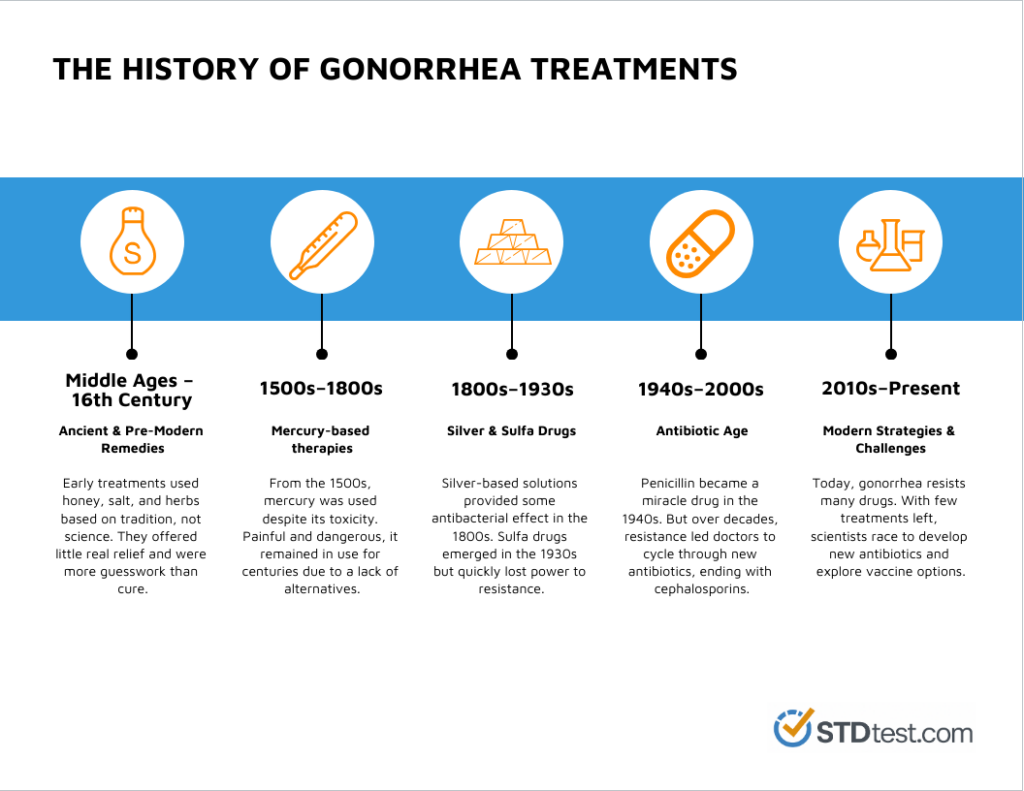
Historically, treatments for gonorrhea were unpleasant and often risky. One dated treatment was to inject the urethra with mercury solutions to disinfect and “wash out” the infection. It was painful, and ran the risk risk of mercury poisoning. Other chemical treatments included silver nitrate, which was applied directly to the affected areas and herbal remedies like balsam of copaiba and cubebs which were thought to have antiseptic and anti-inflammatory properties.
Heat therapy was another popular method, applying heat externally or through heated catheters to “burn out” the infection. In severe cases doctors would cauterize, using heated instruments to sear the urethra. Surgical interventions were attempted to manage complications like abscesses but were rarely successful and often caused more suffering.
During the 20th century, arsenic-based drugs like salvarsan were used. This treatment came with serious side effects. Sulfa drugs in the 30s helped a bit but it wasn’t until the invention of penicillin in the 40s that gonorrhea could be treated effectively and safely.
Evolution of the Term Over Time
The term “gonorrhea” has undergone significant changes over time, reflecting both linguistic evolution and advancements in medical understanding. The word “gonorrhea” is derived from the Greek words gonos, meaning “seed,” and rhoia, meaning “flow.” This etymology refers to the discharge that is a common symptom of the infection.
The term “gonorrhea” has been in use since the 18th century and has become the widely accepted medical term for the infection. This shift from colloquial to formal terminology mirrors the broader trend in medicine towards more precise and scientific language.
Gonorrhea is a type of sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It is a highly contagious infection that can be spread through vaginal, anal, and oral sex. Gonorrhea is a major public health concern due to its high prevalence and potential complications, such as pelvic inflammatory disease (PID) and infertility.
Gonorrhea primarily affects the reproductive organs but infection can spread to the throat, eyes, and rectum. Gonorrhea is identified as an STI, highlighting the need for safe sexual practices and regular testing to help prevent its transmission and address its effects on public health.
Overview of Most Common Symptoms
The most common symptoms include:
- Painful urination
- Pus-like discharge
- Vaginal discharge
- Swollen lymph nodes, particularly around the neck area
Unusual Symptoms of Gonorrhea
Some individuals may experience unusual symptoms that can complicate diagnosis and treatment. These less common symptoms include:
- Rectal Pain or Bleeding: Gonorrhea can infect the rectum, leading to discomfort, bleeding, or discharge.
- Throat Pain or Soreness: Oral sex with an infected partner can result in a gonorrhea infection in the throat, causing pain or soreness.
- Eye Pain or Discharge: Gonorrhea can infect the eyes, leading to pain, redness, and discharge, a condition known as conjunctivitis.
- Skin Rashes or Lesions: In rare cases, gonorrhea can cause skin rashes or lesions.
- Joint Pain or Swelling: Gonorrhea can spread to the joints, causing pain and swelling, a condition known as disseminated gonococcal infection (DGI).
It is essential to seek medical attention if you experience any unusual symptoms, as they can be a sign of a more severe infection.
How Gonorrhea Spreads
Gonorrhea most typically spreads through various forms of sexual contact, including anal sex and vaginal intercourse, affecting the reproductive organs. Understanding transmission can help protect you. Modes of transmission include:
- Sexual Intercourse: The primary way gonorrhea spreads is through oral, anal, or vaginal sex with an infected person.
- Contact with Infected Fluids: Contact with infected bodily fluids, like genital discharge, can lead to infection.
- Mother to Child: During childbirth, an infected mother can pass the bacteria to her baby, which may lead to eye pain or even blindness in the newborn.
- Active Sex Life: Those with multiple sex partners or who engage in sexual contact with an infected person are at higher risk.
- Age Group: Young people, particularly sexually active women younger than 25, are more frequently affected. This demographic is significantly more vulnerable to infection, and routine screening is recommended for sexually active women as a preventative measure.
- Lack of Protection: Not using condoms during intercourse increases the chance of infection.
- Healthcare Access: Areas with limited healthcare services are at higher risk.
- Previous Infections: Having had gonorrhea or other sexually transmitted infections can heighten the risk of reinfection.
- Potential Long-term Health Issues
- Pelvic Inflammatory Disease (PID): This condition affects women’s reproductive organs and can cause severe abdominal and pelvic pain.
- Epididymitis: In men, untreated gonorrhea can result in epididymitis, an inflammation of the tube attached to the testicle, leading to testicular pain and swelling.
- Spread to Blood or Joints: The infection can spread to the bloodstream or joints, causing a condition called disseminated gonococcal infection (DGI). It can result in joint pain, skin sores, and a rash.
- Inflammation: Inflammation in various parts of the body can lead to eye pain, Sore throat, and more.
Impact on Reproductive Health
- Infertility: Untreated gonorrhea in women can cause scarring of reproductive organs, increasing the risk of infertility and pregnancy complications. In men, prolonged infection can reduce fertility.
- Ectopic Pregnancy: Damage to the fallopian tubes from PID increases the risk of ectopic pregnancies, where the fertilized egg implants outside the uterus.
- Infections in Babies: Pregnant women with untreated gonorrhea can pass the infection to their babies during childbirth, causing infections in the baby’s eyes, which might lead to blindness.
Increased Risk of Other Sexually Transmitted Diseases
People with gonorrhea are at an increased risk of contracting other sexually transmitted diseases (STDs), including chlamydia, syphilis, and human immunodeficiency virus (HIV). This increased risk is related to behaviors like unprotected sex, which also raise the chances of contracting other STDs and infections.
It is crucial to practice safe sex and get regular STD testing to reduce the risk of contracting other infections. By understanding the interconnected nature of sexually transmitted diseases, individuals can take proactive steps to protect their sexual health.
Diagnosis of Gonorrhea
Consult the table below to learn about the different testing methods used for diagnosis:
| Testing Method | Description |
| Urine Test | Detects bacteria in urine |
| Swab Test | Samples from the throat, cervix, urethra, or rectum |
| NAAT | Nucleic Acid Amplification Test for accuracy |
The choice of test depends on the symptoms and the areas affected during sexual activity.
Importance of regular screenings
Regular std screenings are crucial for anyone with an active sex life. They help catch infections early, preventing long-term complications. Symptoms of gonorrhea can be mild or mistaken for other issues, like a sore throat or abdominal pain.
Screenings should be a routine part of healthcare for sexually active individuals. This approach protects both the infected person and their sex partners. Regular tests ensure timely gonorrhea treatment, reducing the risk of spreading the infection to others. According to the Centers for Disease Control and Prevention, routine checks can significantly lower the risk of complications associated with untreated gonorrhea.
Treatment Options for Gonorrhea
Antibiotics and Medical Interventions
The primary treatment for gonorrhea involves antibiotics. Medical professionals usually prescribe a combination of antibiotics to combat the bacteria. Below is a table showing common antibiotics used:
| Antibiotic Name | Usage Summary |
| Ceftriaxone | Given as an injection, often a first choice. |
| Doxycycline | Used along with ceftriaxone to handle co-infections. |
| Azithromycin | An alternative for those allergic to other drugs. |
Medical interventions help alleviate associated symptoms like abdominal pain and pus-like discharge. During treatment, it’s crucial to avoid sexual contact to prevent spreading the infection to sexual partners.
Importance of Following Treatment Protocols
Following the prescribed treatment protocol is critical to completely eradicate the infection. Here are some reasons why strict adherence is important:
- Prevent Complications: Untreated gonorrhea can lead to severe health issues, such as pelvic and testicular pain or reproductive organ damage.
- Avoid Resistance: Stopping antibiotics too soon can lead to drug-resistant strains of the infection, complicating future treatment efforts.
- Promote Recovery: Proper treatment reduces the risk of venereal disease and quickens recovery, minimizing symptoms like painful urination and sore throat.
It’s also crucial to inform your healthcare provider of any adverse reactions to the medication. Regular follow-ups may be necessary to ensure the infection is cleared, preventing it from spreading to more sex partners.
Antibiotic Resistance and Future Directions
The rise of antibiotic-resistant gonorrhea is a significant public health concern. The Centers for Disease Control and Prevention (CDC) has reported an increase in antibiotic-resistant gonorrhea cases in recent years. This growing resistance makes it essential to develop new treatment options and strategies to combat the infection.
If left unaddressed, antibiotic-resistant gonorrhea could result in a scenario where the infection becomes untreatable with current antibiotics, leading to heightened morbidity and mortality. Researchers are actively engaged in developing new antibiotics and treatment strategies, including combination therapy and vaccine development, to tackle this issue.
Public health initiatives underscore the importance of completing prescribed treatments and minimizing antibiotic misuse to curb the spread of resistance.
Prevention Strategies
Preventing gonorrhea is important to maintain sexual health and avoid complications such as pelvic pain or inflammatory disease. Below are effective prevention strategies:
- Condoms: Consistently using condoms during sexual intercourse is one of the most effective ways to prevent the spread of the infection.
- Limit Sexual Partners: Reducing the number of sex partners can lower your risk.
- Open Communication: Discuss sexual health with potential partners. Awareness and transparency can help in making informed decisions.
- Regular Testing: Both you and your partner should get tested regularly, especially if you have an active sex life.
FAQs
Can gonorrhea be treated?
Yes, gonorrhea is treatable with antibiotics. However, due to increasing antibiotic resistance, it is important to complete the prescribed treatment and follow up with a healthcare provider to ensure the infection is fully resolved.
What happens if gonorrhea is left untreated?
Untreated gonorrhea can cause major complications complications, such as pelvic inflammatory disease (PID) in women, which can lead to infertility. In men, it can cause epididymitis, a painful condition that can also result in infertility. In rare cases, gonorrhea can spread to the bloodstream, causing disseminated gonococcal infection (DGI), which is life-threatening.
Can you get gonorrhea more than once?
Yes, having gonorrhea once does not provide immunity. You can be reinfected if exposed to the bacteria again, so it’s important to practice safe sex even after treatment.
What is the connection between gonorrhea and other STIs?
Having gonorrhea increases the risk of contracting and transmitting other STIs, including HIV. This is because gonorrhea can cause inflammation and tissue damage, creating easier entry points for other infections.
Is there a vaccine for gonorrhea?
Currently, there is no vaccine for gonorrhea. Researchers are working to develop one, but for now, prevention relies on safe sexual practices and regular screenings.
Are there any myths about gonorrhea?
Yes, common myths include the idea that you can catch gonorrhea from toilet seats or casual contact—this is not true. Another misconception is that gonorrhea always causes noticeable symptoms, but many cases are asymptomatic.
Can you get gonorrhea through oral sex or anal sex?
Yes, gonorrhea can be transmitted through oral sex and anal sex. Engaging in oral sex with an infected person can lead to a gonorrhea infection in the throat, often resulting in symptoms like a sore throat or throat pain. Similarly, anal sex with an infected partner can cause the infection to spread to the rectum, leading to symptoms such as rectal pain, discharge, or bleeding. Practicing safe sex by using condoms and dental dams can help reduce the risk of spreading gonorrhea through these types of sexual contact.
